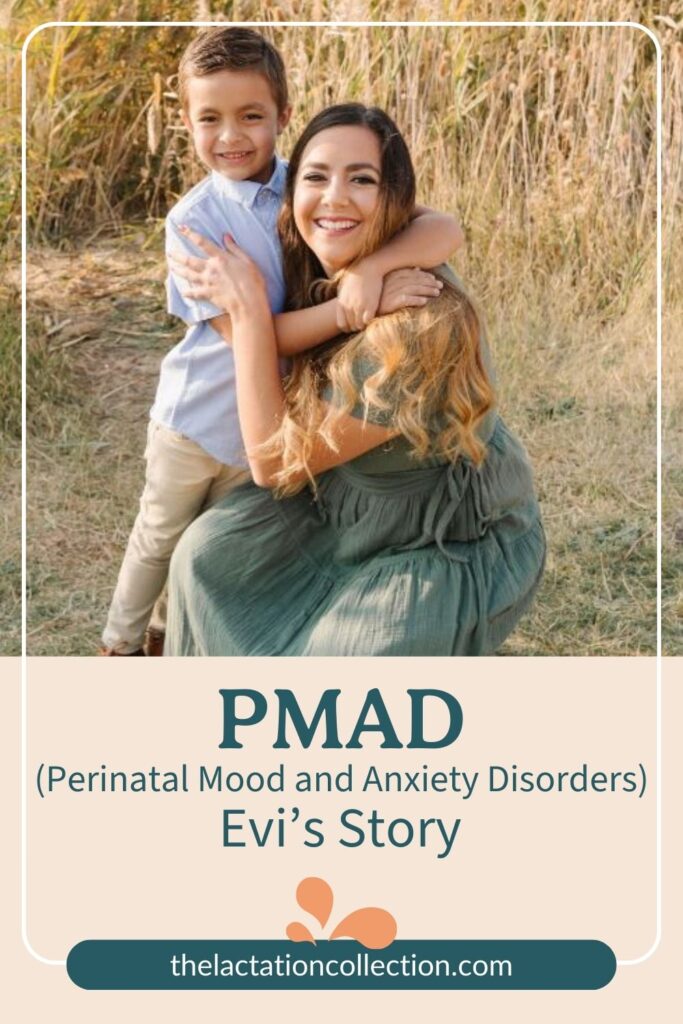
The following story shows what PMADs (Perinatal Mood and Anxiety Disorders) can look like. No experience is the same. The information shared in this post is in no way a substitute for professional diagnosis or treatment. Below you will read the experience of Evi Figgat.

The Perfect Storm
I first experienced perinatal mood and anxiety disorders (PMADS) following my son’s birth six years ago. I didn’t understand then, but my life had presented me with the perfect storm of pre-disposers and the odds completely stacked against me.
A couple of years before my son’s birth, I had been diagnosed with depression. I struggled to breastfeed due to polycystic ovarian syndrome. I was getting even less sleep than typical because I pumped for hours after feedings, desperately trying to get more milk (this is when I should’ve turned to an ICBLC like Anna). Then, when my son was six weeks old, my husband lost his job—effective immediately. I was devastated. We picked up all of our belongings and left the state we had resided in for six years, and moved to California. All of these events and health issues predispose women to PMADS.
Previous mental health struggles, difficulty breastfeeding, sleep deprivation, job loss/joblessness, and moving are common triggers for PMADs. I wish I had known the factors that predispose you to PMADs.
My depression and anxiety often manifested as rage, difficulty leaving the house, emotional numbness, and sleeping at strange times excessively. I would find myself yelling, really yelling at absolutely everyone in my personal circle. I could hear the words leaving my mouth and felt zero control. I’d sleep whenever my son slept, which was fine for a little while but soon, I prioritized sleep over everything. Situations that should’ve made me happy, like hanging out with friends, made me feel nothing, and that’s assuming that I could get out of the house. Many times I felt overwhelmed by the thought of anything outside of the home.
I felt a tremendous amount of pressure not to burden anyone and do it all on my own. I spiraled downward for six months. Finally, when I was six months postpartum, after a long night of working on my graduate school work, I experienced postpartum psychosis. It terrified me. I called my husband, and he and my mom were at my side within thirty minutes. I wish I could say things immediately got better, but they didn’t. It was time for the hard work to start.
Getting Help
I started seeing a psychiatrist twice a week. She placed me on medication immediately, and I had strict boundaries around sleep. I had to let go of the idea of burdening others, so I let go of guilt around the idea of my mom helping me and allowed my husband to carry some of the weight with parenting and household tasks. Things did get better, slowly. However, it wasn’t until I was about a year postpartum that things felt like they should. I immensely enjoyed motherhood, especially once things got better.
My husband and I decided together that we wouldn’t have another child until I felt fully emotionally and physically ready, and we had to have a postpartum game plan.
A Second Baby
Fast forward to three years postpartum; I felt ready. I hadn’t experienced anxiety or depression in months. I dutifully took my meds but felt prepared to drop the medication that isn’t advised for pregnancy (Seroquel). I had an extremely successful pregnancy, birth, and immediate postpartum. In my mind, I was the poster child for hope after severe PMADS.
I made it until March 2020 (nine months postpartum). Right as the pandemic hit, my daughter contracted RSV, then COVID, and had an autoimmune response called Kawasaki’s Syndrome, which landed her in the pediatric intensive care unit for two weeks. When we left the hospital, the world was shut down. We had closed on our first home while my daughter was in the hospital. That’s when the pressure became too much, and PMADS re-entered my life.
This time, though, we knew what to do.

Hope
Within the first week of feeling the first symptoms, I was on medication and regularly seeing a therapist. Okay, “seeing” is a strong word. I was video-chatting with her (thanks, 2020). Regardless of how help showed up in my life, it showed up because my husband and I knew what we were looking at and knew we needed to quickly take action not to allow it to take control of my life.
To my great pleasure, it didn’t.
I worked my way through postpartum depression and anxiety a second time (plus, no psychosis this time!). I’d be lying if I didn’t say that I still have hard days at nearly two years postpartum. That’s okay. I move forward each day with hope.
Postpartum depression, anxiety, or psychosis don’t have to be the end for you. These PMADs don’t have to be your forever. Find help. Find hope.
You’ve got this, mama.
If you feel like you’re experiencing PMADS, reach out for help. You don’t have to suffer alone. If you’re local, we recommend Maternal Mental Health Utah, PSI Utah (there are chapters throughout the world), or The Emily Effect. If you’re experiencing any thoughts of self-harm, reach out to 800-273-8255, or use their chat function.